What is GERD?
The stomach normally secretes acid that is essential in the digestive process. This acid helps in breaking down the food during digestion. When there is excess production of acid by the gastric glands of the stomach, it results in the condition known as acidity, dyspepsia, heartburn.
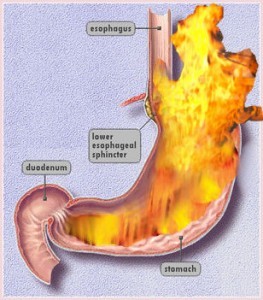
Heartburn is burning sensation in mid chest or throat that’s caused by digestive juice acid rising up from stomach to the food pipe or esophagus It’s a common symptom of the condition called gastroesophageal reflux disease or GERD, also called acid reflux or acid regurgitation. Occasional reflux is common , reflux more than twice a week is GERD.
Symptoms:
Heartburn. Most likely to occur in connection with the following activities:
- Eating a heavy meal
- Bending over
- Lifting
- Lying down, particularly on the back
Dyspepsia.
- Pain and discomfort in the upper abdomen
- A feeling of fullness in the stomach
- Nausea after eating
Regurgitation. feeling of acid backing up in the throat. Sometimes acid regurgitates as far as the mouth and can be experienced as a “wet burp.”
Less Common Symptoms
Elderly patients with GERD often have less typical symptoms than do younger people. Most children under 12 years with GERD, and some adults, may have GERD without heartburn. Instead, they may have dry cough, asthma symptoms, or trouble swallowing
Chest pain-
Chest pain is a common symptom of GERD. It is very important to differentiate it from chest pain caused by heart conditions.
Symptoms in the Throat-
- Acid laryngitis. A condition that includes hoarseness, dry cough, the sensation of having a lump in the throat, and the need to repeatedly clear the throat.
- Trouble swallowing. In severe cases, patients may choke or food may become trapped in the esophagus, causing severe chest pain. This may indicate a temporary spasm that narrows the tube, or it could indicate serious esophageal damage or abnormalities.
- Chronic sore throat
- Persistent hiccups
Coughing and Respiratory Symptoms. Airway symptoms, such as coughing and wheezing, may occur.
Chronic Nausea and Vomiting. Nausea or in rare cases vomiting can occur.
What causes GERD?
When we eat, food travels from mouth to stomach through a tube called the gullet or esophagus. At the lower end of the esophagus is a small ring of muscle called the lower esophageal sphincter (LES) which acts like a one-way valve, allowing food to pass through into the stomach. Normally, it prevent back-flow of stomach juices (acid)) into the esophagus. GERD occurs when the LES does not function properly allowing acid to flow back and burn the lower esophagus. This irritates and inflames the esophagus, causing heartburn and eventually may damage the esophagus. Research shows that in people with GERD, the LES relaxes while the rest of the esophagus is working. There may be Impaired Stomach Function or Motility Abnormalities.About 30 – 40% of reflux may be hereditary.
What contributes to GERD?
Common foods that can worsen reflux symptoms include
- citrus fruits
- chocolate
- Soda
- drinks with caffeine or alcohol
- fatty and fried foods
- garlic and onions
- mint flavorings
- spicy foods
- Tomato
Many other factors can also play a role in triggering heartburn and causing GERD
- Overeating. Stomach remains distended when there are large quantities of food in it. The more your stomach stays distended, the more likely the LES won’t close properly. When it doesn’t close, it can’t prevent food and stomach juices from rising back up into the esophagus.
- Eating habits. Eating too rapidly, eating while lying down or too close to bed time can be a heartburn trigger.
- Smoking. Smoking cigarettes is another potential cause of heartburn.
- Hiatal hernia. Your diaphragm is a muscular wall that separates your stomach from your chest. It helps the LES keep stomach acid where it belongs. When the LES and the upper part of the stomach move above the diaphragm you develop a hiatal hernia. The hernia makes acid reflux, which causes heartburn, more likely.
- Obesity or overweight. Research suggests that being obese or overweight can be a trigger for heartburn and reflux disease.
- Pregnancy. Pregnant women are particularly vulnerable to GERD in their third trimester, as the growing uterus puts increasing pressure on the stomach. Heartburn in such cases is often resistant to dietary interventions and even to antacids.
- Medicines. Common medications taken for other problems can increase the likelihood of heartburn. That includes medicines used to treat asthma, high blood pressure, heart problems, arthritis or other inflammation, osteoporosis, anxiety, insomnia, depression, pain, Parkinson’s disease, muscle spasm, or cancer.
- Exercise. Increased pressure on the abdomen can increase the risk of acid reflux. Weightlifters had the most heartburn and acid reflux. Runners had milder symptoms and less reflux than weightlifters.
How is GERD treated?
If you have had symptoms of GERD and have been using antacids or other over-the-counter reflux medications for more than 2 weeks visit a gastroenterologist
Depending on the severity of your GERD, treatment may involve one or more of the following lifestyle changes, medications, or surgery.
General Measures – Self-Care
Some dietary and lifestyle tips for heartburn relief-
- Avoid trigger foods. Classic GERD triggers include chocolate, coffee, cols, alcohol, peppermint, citrus juices, and tomatoes. The exact food triggers vary from person to person
- Eat smaller meals. Avoid stuffing yourself. Try more frequent smaller meals. Don’t escape breakfast
- Don’t eat too quickly
- Don’t eat before bed. You shouldn’t eat two to three hours before bed. Not eating gives your stomach time to empty before you lie down.
- Loosen your belt. Tight belts or pants can aggravate your GERD symptoms. Wear looser clothing, especially at night.
- Prop up the bed. When you stick blocks under the head of your bed and raise it 6 to 8 inches, gravity will prevent the acids in your stomach from flowing into the esophagus during the night.
- Lose weight. If you’re obese, aiming for a 10% weight loss is always a good idea.
- Evaluate your other medications. Many common medications — aspirin and other NSAID painkillers, along with some drugs for high blood pressure — can make GERD worse.
- Stop smoking.
Medications for GERD
Antacids, are usually the first drugs recommended to relieve heartburn and other mild GERD symptoms.
Foaming agents, work by covering your stomach contents with foam to prevent reflux.
H2 blockers, ranitidine decrease acid production. provide short-term relief and are effective.
Proton pump inhibitors omeprazole lansoprazole pantoprazole , rabeprazole and esomeprazole are more effective than H2 blockers and can relieve symptoms and heal the esophageal lining.
Prokinetics help strengthen the LES and make the stomach empty faster. This group includes bethanechol (Urecholine) and metoclopramide (Reglan). Metoclopramide also improves muscle action in the digestive tract. Prokinetics have frequent side effects that limit their usefulness—fatigue, sleepiness, depression, anxiety,
What if GERD symptoms persist?
If your symptoms do not improve with lifestyle changes or medications, you may need additional tests.
Barium swallow radiograph uses x rays to help spot abnormalities such as a hiatal hernia and other structural or anatomical problems of the esophagus. With this test, you drink a solution and then x rays are taken. The test will not detect mild irritation, although strictures—narrowing of the esophagus—and ulcers can be observed.
Upper endoscopy is more accurate than a barium swallow radiograph. The doctor may spray your throat to numb it and then, will slide a thin, flexible plastic tube with a light and lens on the end called an endoscope down your throat. The endoscope allows the doctor to see the surface of the esophagus and search for abnormalities.
The doctor also may perform a biopsy. The tissue is then viewed with a microscope to look for damage caused by acid reflux and to rule out other problems if infection or abnormal growths are not found.
pH monitoring examination through a small tube into the esophagus or a tiny device to the esophagus that will stay there for 24 to 48 hours. when and how much acid comes up into your esophagus is measured. This test can be useful if combined with a carefully completed diary—recording when, what, and amounts the person eats—which allows the doctor to see correlations between symptoms and reflux episodes.
Surgery For GERD
Surgery is an option when medicine and lifestyle changes do not help to manage GERD symptoms. Surgery may also be a reasonable alternative to a lifetime of drugs and discomfort. With the new minimally invasive approach, surgery is now a viable initial therapy and is safe and effective in people of all ages, including infants.
Nissen Fundoplication is surgery to repair hiatal hernia and is surgical treatment for GERD. Upper part of the stomach is wrapped around the LES to strengthen the sphincter, prevent acid reflux, and repair a hiatal hernia.
Endoscopic techniques. In one endoscopic method for treating GERD, an instrument is inserted that delivers an electrical current to the lower esophageal sphincter. This results in scarring which tightens the sphincter. In a second method, sutures are placed in the sphincter to tighten the sphincter
What are the long-term complications of GERD?
Having heartburn more than occasionally can reduce your quality of life. It can affect not just what you eat, but how you sleep and what activities you do.
Chronic GERD that is untreated can cause serious complications. Inflammation of the esophagus from refluxed stomach acid can damage the lining and cause bleeding or ulcers—also called esophagitis. Scars from tissue damage can lead to strictures—narrowing of the esophagus—that make swallowing difficult.
Some people develop Barrett’s esophagus, in which cells in the esophageal lining take on an abnormal shape and color. Over time, the cells can lead to esophageal cancer, which is often fatal.
Studies have shown that GERD may worsen or contribute to asthma, chronic cough, and pulmonary fibrosis.
Ref: www.digestive.niddk.nih.gov National Digestive Diseases Information